Introduction
A considerable number of adults, particularly those aged 50 and above, frequently encounter the discomforts of varicose veins and leg cramps, highlighting these conditions as prevalent health concerns. Although these ailments are typically viewed as distinct and unrelated, emerging evidence suggests a noteworthy link between them that deserves further investigation. Let’s explore the intricate connection between varicose veins and leg cramps, shedding light on the potential ways they are interconnected, understanding the health repercussions they entail, and exploring effective strategies for symptom management and relief.
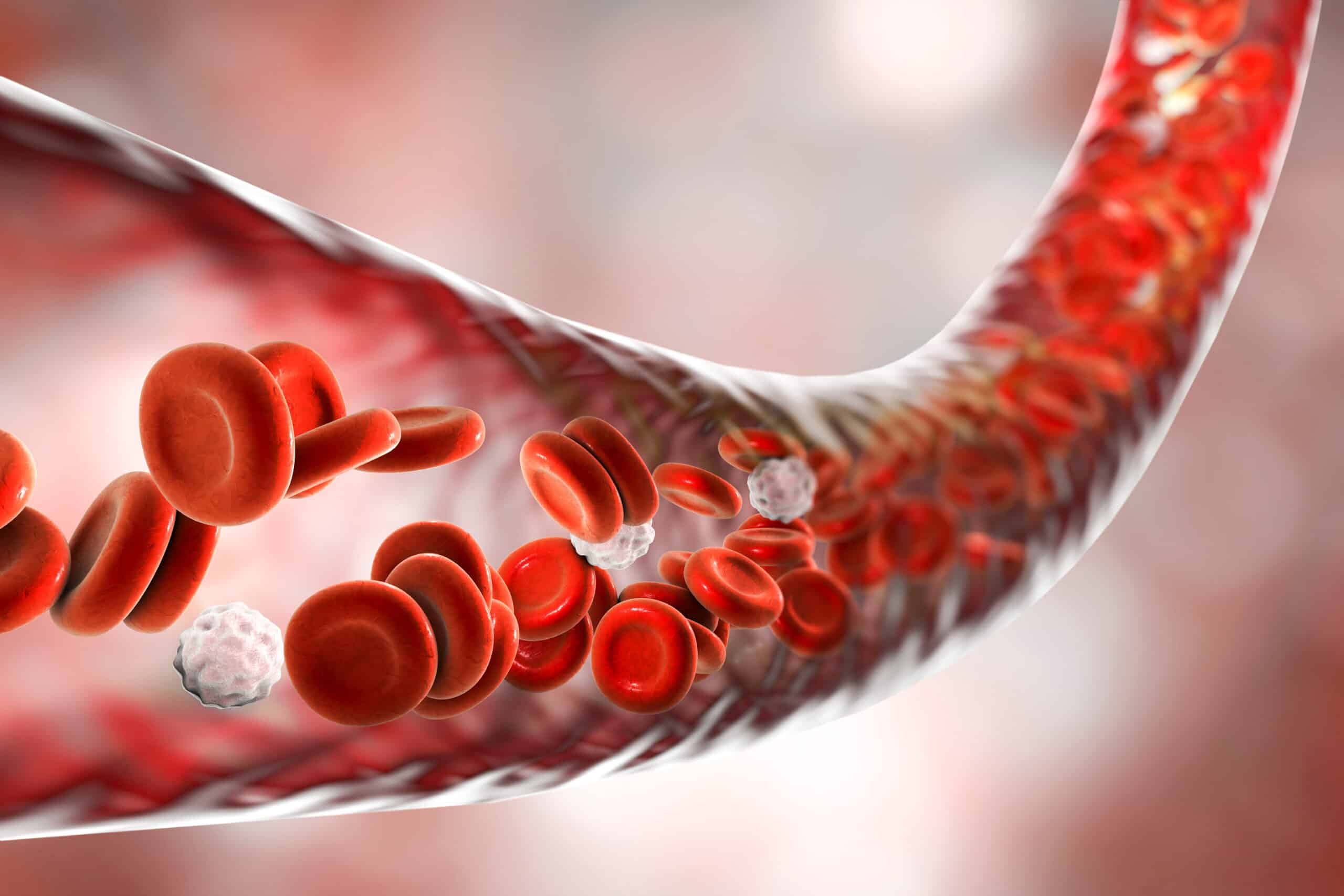
Understanding Varicose Veins
Varicose veins manifest as large, swollen, and intricately twisted vessels, frequently exhibiting a blue or dark purple hue. This condition arises due to malfunctioning valves within the veins, which leads to the improper flow of blood, either in the reverse direction or causing it to accumulate. Predominantly affecting the legs and feet, varicose veins become more prevalent in these areas as the act of standing and walking in an upright position significantly escalates the pressure exerted on the veins situated in the lower part of the body.
Symptoms of Varicose Veins
- Visible Veins
- Aching or heavy legs
- Swelling
- Pain after prolonged sitting or standing often
- Itching around the veins
- Burning sensations, throbbing pain, muscle cramps, and swelling in the lower legs
- Hardening of the vein
- Ulcers or sores
- Bleeding
Leg Cramps: A Painful Intruder
Leg cramps involve abrupt and involuntary contractions of the muscles, typically resulting in intense pain. They can last from a few seconds to several minutes.
While they can occur in any part of the leg, they are most commonly experienced in the calves. These cramps can disrupt sleep and affect the quality of life.
Common Causes of Leg Cramps
- Muscle overuse
- Dehydration
- Mineral deficiencies
- Poor circulation
- Nerve compression
- Medications
- Age
- Pregnancy
- Medical conditions
- Inactivity
The Relationship Between Leg Cramps and Varicose Veins
The link between varicose veins and leg cramps is rooted in the problems of circulation and venous insufficiency that varicose veins frequently represent. Far from being merely aesthetic issues, varicose veins signal deeper venous health problems that can majorly affect one’s quality of life through various discomforts and pains, such as leg cramps. Here’s how these two conditions are interconnected:
- Impaired Circulation: Blood pools in the veins due to inadequate blood return from the legs to the heart, which is indicated by varicose veins. Cramping may result from this decreased transport of nutrients and oxygen to the muscles.
- Venous Hypertension: Blood pooling due to varicose veins increases venous pressure, causing fluid to leak into surrounding tissues, leading to swelling. This swelling can pressure muscles and nerves, resulting in cramps.
- Inflammation: Varicose veins can trigger an inflammatory response, exacerbating leg discomfort and contributing to cramps.
- Nutrient Deficiencies: Impaired blood flow from varicose veins can affect the distribution of essential nutrients and electrolytes, such as potassium, calcium, and magnesium, necessary for muscle function and health, potentially causing cramps.
- Mitigating Factors: Lifestyle adjustments (diet, hydration, exercise), along with medical interventions like compression therapy and surgical options for varicose veins, can help manage and reduce the symptoms of both varicose veins and leg cramps.
- Treatment and Management: Addressing leg cramps with stretching, proper hydration, and mineral supplementation, in addition to treating varicose veins, can offer significant relief. Consulting a healthcare provider for severe or persistent symptoms is crucial for a comprehensive treatment approach.
Understanding the connection between varicose veins and leg cramps is crucial for managing both conditions effectively. Treatment options for varicose veins, such as lifestyle changes, compression therapy, and in some cases, surgical interventions, can help reduce the incidence of leg cramps.
Moreover, addressing leg cramps directly through stretching, adequate hydration, and supplementation with essential minerals can provide relief. If you experience severe or persistent leg cramps and varicose veins, consulting with a healthcare provider is essential for a comprehensive evaluation and tailored treatment plan.
Managing Varicose Veins and Leg Cramps
Managing varicose veins and leg cramps effectively involves a combination of lifestyle modifications, self-care measures, and potentially medical treatment, depending on the severity of the conditions. Here are strategies to help manage these issues:
Lifestyle Modifications
- Regular Exercise: Engage in activities that improve circulation and strengthen the muscles in your legs, such as walking, swimming, or cycling. Exercise can help pump blood back towards the heart and reduce symptoms.
- Maintain a Healthy Weight: Excess weight can increase the pressure on your veins, exacerbating varicose veins and associated symptoms like leg cramps. A balanced diet and frequent exercise will help you reach your goal weight.
- Elevate Your Legs: Several times a day, raising your legs above your heart can help to increase circulation and lower vein pressure.
- Avoid Prolonged Standing or Sitting: Frequently shift positions to promote blood flow. If you must stand or sit for extended amounts of time at work, take frequent breaks to move around, or think about utilizing a footrest to raise your legs slightly when seated.
Self-care Measures
- Stay Hydrated: Staying hydrated can help avoid cramps by preserving the function of your muscles and nerves.
- Dietary Adjustments: Ensure your diet includes sufficient amounts of potassium, magnesium, and calcium, as deficiencies in these minerals can contribute to leg cramps.
- Compression Stockings: Wearing graduated compression stockings during the day can help squeeze your legs, improving blood flow and reducing pain and swelling associated with varicose veins.
Medical Treatments
- Sclerotherapy: In order to scar and seal the varicose veins, a solution must be injected into them. The treated veins disappear with time.
- Endovenous Laser Therapy (EVLT) or Radiofrequency Ablation (RFA): These treatments use heat to close off varicose veins, diverting blood flow to healthier veins.
- Vein Stripping and Ligation: In more severe cases, surgery may be required to remove or tie off the affected veins.
When to See a Doctor
- If you’re experiencing severe or persistent leg cramps and varicose veins that interfere with your daily life.
- If you notice skin changes, ulcers, or a sudden increase in swelling or pain in your legs.
To assess your problem and go over the best course of therapy, it is imperative that you speak with a healthcare professional. A specialist, such as a vascular surgeon or a phlebologist, can offer advice tailored to your specific situation. Managing varicose veins and leg cramps effectively not only improves your quality of life but can also prevent potential complications.
Conclusion
While varicose veins and leg cramps may be related, recognizing the signs early on, along with implementing lifestyle modifications and seeking medical treatment, can greatly reduce symptoms and enhance one’s quality of life. At Idunn Clinic in Torrance, CA, we proudly offer Sclerotherapy, a minimally invasive procedure that not only addresses varicose and spider veins by collapsing and fading them over time but also alleviates associated leg cramps by rerouting blood to healthier veins, enhancing leg appearance with noticeable results in just a few sessions. Revitalize and transform your legs with Sclerotherapy—effortlessly banishing varicose veins and alleviating leg cramps to enhance your appearance and comfort, granting you the freedom and confidence with every step you take!